Get Your Nerve Pain Treated Sooner & Save 77% Off Your Consultation
Understanding and Easing Nerve Pain
If you’re suffering from nerve pain, the only thing you want is for that pain to stop. It stands to reason.
The problem for many people in that situation is that the drugs they take are strong and have undesirable side effects.
The medicine may temporarily mask the pain but it also affects quality of life in other ways, such as impairing mental clarity or causing severe drowsiness.
The underlying cause of the pain often goes untreated, meaning that the pain returns and the cycle of painkilling drug dependency continues.

A better approach to nerve pain treatment is a multi-disciplinary one that combines manual nerve release with other interventions that also treat the underlying cause of the nerve pain. For example, if you have diabetic neuropathy the diabetes must be addressed, and manual therapy applied to areas where mechanical nerve tension is also contributing to the problem.
Leave your name and number in the form below or Call Us Now On 01234 340 317
What is Nerve Pain?
Nerve pain (also called “neuropathic pain”) occurs when the somatosensory system is either damaged or affected by disease.
The somatosensory system is part of the sensory nervous system. Without it, we would not be able to feel the sensations of touch, pressure, pain, temperature, position, movement, and vibration arising from nerves in the muscles, joints, and skin.
Nerve pain can severely impact quality of life, affecting the ability to sleep properly, perform normal day-to-day tasks, and to work. It can even lead to depression and anxiety.
Pain often affects the extremities like the hands first, which complicates tasks we take for granted like writing or brushing teeth. It can also weaken muscles (due to inactivity) and lead to problems with balance, which is especially serious for elderly people.
Without specialist attention, the pain can be severely debilitating. It is experienced in many different ways, from intermittent stabbing pain to tingling or burning.
Nerve pain is often worse when the body is in certain positions or undergoing certain activities, such as walking or simply standing up or lying down.
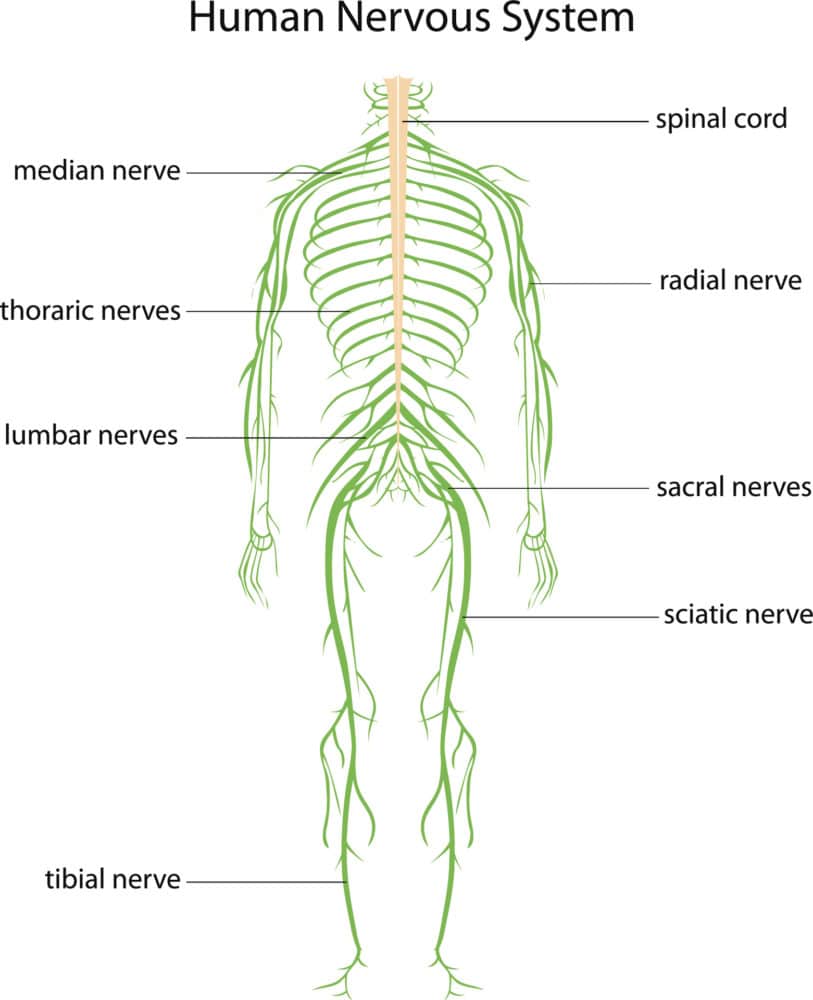
Left untreated, it will generally worsen, spreading from the feet and hands to the legs and arms, for instance.
Nerve pain already affects up to 10 percent of the population in the UK. Because of our ageing population, the growth of chronic diseases like diabetes, and improved survival rates from cancer therapy, the problem is likely to get worse in the coming years if not addressed.
How is nerve pain typically treated?
At present, the approach from the medical establishment towards nerve pain is not adequately addressing the growing problem.
Nerve pain can be complex, with a variety of symptoms presenting in patients. Over-medicating has often led to poor outcomes for the patient in terms of quality of life. Many patients have to make multiple visits to medical centres to get relief from their pain, and still that approach doesn’t correct the underlying cause of the problem.
Like all pain, nerve pain should be considered as the body’s way of warning you that something is wrong. There is an underlying problem that is causing the pain.
Nerve damage can mean that the body’s ‘warning system’ malfunctions. You may feel pain but the body is sending ‘false signals’, not really reflecting the underlying cause; or numbness may mean that you feel no pain at all at the site of an injury.
This makes nerve pain extra-difficult to diagnose and treat.
Most people start with over-the-counter painkillers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, analgesics (such as acetaminophen) or prescription medicines.
Patients may also try a variety of creams, ointments, oils, gels, or sprays to ease the pain.
Usually, none of these methods cause any harm in the short term but they may be ineffective, and other problems can arise if you become reliant on the painkillers. Long-term use however increases the potential for harm to develop.
This is especially the case for stronger prescription medications like depression and epilepsy drugs that are often prescribed for nerve pain.
Many of these have questionable results and may result in severe side effects, including drowsiness, mental impairment, nausea, and others.
Leave your name and number in the form below or Call Us Now On 01234 340 317
A better approach to treating nerve pain
Managing and treating nerve pain needs to become more personalized and less dependent upon medication to become more effective.
This means understanding the cause of your pain.
Patients themselves can help by noting the nature of the pain, its progression over time, the precise sensations it causes and how long it’s been affecting them.
While new medications are being developed, the track record is not particularly encouraging on this front, which means that we also need to consider other treatments for nerve pain.
Some of these are summarised below.

Interventional therapies
These include nerve blocks and surgical procedures that deliver medication to targeted areas causing the pain or modifying the nerve structures. However, these treatments have been associated with complications such as infections, and surgical scarring can cause significant problems later on even if the patient does get some short-term relief.
Neural blockade and steroid injections
Steroidal injections may help ease the pain temporarily but there are limits to how many of these can be administered and do not address the root cause of the pain. They appear to have no longer-term benefit.
Spinal cord stimulation
Some long-lasting results have been achieved with stimulation of the spinal cord. This is cost-effective and relatively safe and has been shown to be effective for some types of nerve pain, in combination with specific lifestyle modifications.
Neurostimulation
Neurostimulation of nerve fibres outside the spinal cord has been reported to provide pain relief in various cases of chronic nerve pain and further trials are being conducted.
Deep brain stimulation
This has been shown to be effective in some patients with particular types of nerve pain but its use remains controversial.
Physical and occupational therapies
Complementary treatments that involve physical therapy, exercise and movement representation techniques have also suggested some benefit for individuals suffering nerve pain.
This includes mirror therapy and motor imagery, which involve the use of observation and/or imagination of normal pain-free movements.
Acupuncture and supplements such as vitamin B-12 may also be of use in treatment.
Psychological therapies
Psychological interventions for nerve pain like cognitive-behavioral therapy (CBT) are increasingly being trialled.
They are designed to promote the management and reduction of the effects of pain and may provide a useful additional therapy where other interventions have not worked.
Diet and exercise
It’s always worth adding that taking regular exercise, maintaining a healthy weight, and eating a nutritional diet may help to ease nerve pain in the longer term, as well as bringing other health benefits to your life.
When weighing up all the various options for treating nerve pain, there is no one solution that stands out.
A personalised approach using a combination of therapies may offer the most relief for patients but one thing is for certain: reliance on drugs alone is rarely a sustainable option.
Spine, Body & Health Treatment & Therapy
Getting your Nerve Pain treated is simple. It all starts with a consultation with one of our spinal specialists at Spine, Body & Health.
This consultation is, in our opinion, the best in the area as it gives complete clarity and understanding about why you are truly in pain. With this information we can then give you a structured and personalised recommendation of care to help treat your nerve pain.
Click the button below to start your journey with Spine, Body & Health.
Save 77% Off Your Consultation
Click the Button or Call Us Now on 01234 340317
Book Your Consultation Today!
If you’re suffering then we want to help.
Fill out the form to the right and one of our team will contact you to get you booked in for your initial consultation.
They will be on hand to answer any questions you have and talk you through how you can save up to 77% off the consultation fee, instantly.
We look forward to meeting you and helping you on your journey!
Dr. Peter Olsson
Fill out this form to receive health news, exclusive discounts and learn how to book your consultation.
We will take a £10 deposit to secure your consultation.
References
Luana Colloca et al. Neuropathic pain. Nat Rev Dis Primers. ; 3: 17002. doi:10.1038/nrdp.2017.2.
Attal N, Lanteri-Minet et al. The specific disease burden of neuropathic pain: results of a French nationwide survey. Pain. 2011; 152:2836–2843. [PubMed: 22019149]
Torrance N. et al. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain. 2006; 7:281–289. [PubMed: 16618472]
Emery EC, Luiz AP, Wood JN. Nav1.7 and other voltage-gated sodium channels as drug targets for pain relief. Expert Opin Ther Targets. 2016; 20:975–983. [PubMed: 26941184]
Cruccu G, et al. EFNS guidelines on neurostimulation therapy for neuropathic pain. Eur J Neurol. 2007; 14:952–970. [PubMed: 17718686]
Dworkin RH, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013; 154:2249–2261. [PubMed: 23748119]
Mekhail NA, et al. Retrospective review of 707 cases of spinal cord stimulation: indications and complications. Pain Pract. 2011; 11:148–153. [PubMed: 21371254]
Eldabe S, Buchser E, Duarte R. V Complications of spinal cord stimulation and peripheral nerve stimulation techniques: a review of the literature. Pain Med. 2016; 17:325–336. [PubMed: 26814260]
Bhatia A, Flamer D, Shah PS. Perineural steroids for trauma and compression-related peripheral neuropathic pain: a systematic review and meta-analysis. Can J Anaesth. 2015; 62:650–662. [PubMed: 25744141]
Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. [PubMed: 23598728]
Chou R, et al. Epidural corticosteroid injections for radiculopathy and spinal stenosis: a systematic review and meta-analysis. Ann Intern Med. 2015; 163:373–381. [PubMed: 26302454]
North RB, et al. Spinal cord stimulation versus re-operation in patients with failed back surgery syndrome: an international multicenter randomized controlled trial (EVIDENCE study). Neuromodulation. 2011; 14:330–335. [PubMed: 21992427]
Kumar K, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132:179–188. [PubMed: 17845835]
Simpson EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J. Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation. Health Technol Assess. 2009; 13:1–154.
Kumar K, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008; 63:762–770. [PubMed: 18981888]
Kemler MA, De Vet HC, Barendse GA, Van Den Wildenberg FA, Van Kleef M. The effect of spinal cord stimulation in patients with chronic reflex sympathetic dystrophy: two years’ follow-up of the randomized controlled trial. Ann Neurol. 2004; 55:13–18. [PubMed: 14705107]
Krames ES. The role of the dorsal root ganglion in the development of neuropathic pain. Pain Med. 2014; 15:1669–1685. [PubMed: 24641192]
Petersen EA, Slavin KV. Peripheral nerve/field stimulation for chronic pain. Neurosurg Clin N Am. 2014; 25:789–797. [PubMed: 25240665]
Dobson JL, McMillan J, Li L. Benefits of exercise intervention in reducing neuropathic pain. Front Cell Neurosci. 2014; 8:102. [PubMed: 24772065]
Kluding PM, et al. The effect of exercise on neuropathic symptoms, nerve function, and cutaneous innervation in people with diabetic peripheral neuropathy. J Diabetes Compl. 2012; 26:424–429.
Smart KM, Wand BM, O’Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database Syst Rev. 2016; 2:CD010853. [PubMed: 26905470]
Thieme H, Morkisch N, Rietz C, Dohle C, Borgetto B. The efficacy of movement representation techniques for treatment of limb pain — a systematic review and meta-analysis. J Pain. 2016; 17:167–180. [PubMed: 26552501]
Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012; 11:CD007407. [PubMed: 23152245]
Disclaimer: Every effort has been made to accurately represent all services provided by Spine, Body & Health. There is no guarantee that you will get specific results by working with us. Examples on this site are not to be interpreted as a promise or guarantee.
Your level of success in attaining the results claimed on this site and by our staff depend on several factors, such as your background, motivation, commitment, and actions. Since these factors differ according to individuals I cannot guarantee your success, nor am I responsible for any of your actions. Results may vary.
© Copyright 2023 Spine, Body & Health. All Rights Reserved.
